Crohn’s Disease
Crohn’s Disease is one of a group of conditions called Inflammatory Bowel Disease (IBD) which causes the intestines to become inflamed (red and swollen). Two major types of IBD are Crohn’s Disease and Ulcerative Colitis. Ulcerative Colitis affects the large intestine (colon) whereas Crohn’s disease can occur in any part of the intestines.
Crohn’s disease can involve any part of the gastrointestinal tract from the mouth to the anus but most commonly affects the small and large bowel, including the lower small intestine (ileum).
There may be areas of healthy intestine between areas of diseased intestine (“skipped lesions”). Within a diseased section, Crohn’s disease can affect entire thickness of the intestinal wall and not just the lining.
SYMPTOMS OF CROHN’S DISEASE
Gastrointestinal 
Image: patients with Crohn’s can have aphthous ulcers involving mouth.
Many people with Crohn’s disease have symptoms for years prior to the diagnosis, as it can be difficult to diagnose the disease. The peak onset is between 15 and 30 years of age, affecting patients from both sexes equally. A much smaller number of patients are diagnosed with Crohn’s between the ages of 50 and 70 years but the disease can occur in people of any age. Because of the ‘patchy’ nature of the gastrointestinal disease and the depth of tissue involvement, initial symptoms can be non-specific and more subtle than those of Ulcerative Colitis. People with Crohn’s disease experience fluctuations in their symptoms, with recurring periods of flare-ups and remission.
- Abdominal pain may be the initial symptom of Crohn’s disease, and often is associated with diarrhoea or loose stools. The bowel motions may or may not be bloody, and can contain mucous. The nature of the diarrhoea in Crohn’s disease depends on the segment or location of the small intestine or colon involved. Inflammation of the very last part of the small bowel that joins with the large bowel is called “Ileitis”. Ileitis typically results in large-volume and watery stools. “Colitis” (inflammation of the colon) may result in a smaller volume of faeces but often in higher frequency. In some patients with severe disease, it is not unusual to have more than 20 bowel movements per day. Some patients may need have bowel motions at night. Macroscopic bleeding (visible with the naked eye) in the faeces is less common in Crohn’s Disease than in Ulcerative Colitis, although if the disease affect the colon, the pattern of bleeding is often indistinguishable. Bloody bowel movements can spontaneously resolve, and may be bright or darker red in colour. In the setting of severe Crohn’s colitis, the volume of bleeding may be copious and urgent Gastroenterologist review is recommended. Flatulence and abdominal bloating is not uncommon, and is caused by distention of the colon by gases that are produced by colonic bacteria by the process of fermentation of undigested foods (see Hydrogen Breath Testing; Fructose and Lactose mal-absorption; FODMAPs.
- Symptoms caused by intestinal stenosis / strictures (intestinal obstruction or narrowing of the intestinal wall) are common in Crohn’s Disease. Strictures can cause abdominal pain and weight loss which is a late symptom and should always be investigated by a Gastroenterologist. Abdominal pain is often most severe in areas where the stenosis are found. Persistent vomiting and nausea may signal obstruction occurring in pylorus (the part joining the stomach and small bowel), or duodenum (the first 25-30cm of the small bowel). Recurrent vomiting should not be ignored, nor should it be attributed to Irritable Bowel Syndrome, as it can delay correct diagnosis.
- Perianal discomfort may also be prominent in Crohn’s Disease. Itchiness or pain around the anus may be suggestive of inflammation. Fistulae (abnormal channels connecting different loops of intestine to itself, or to the skin and other internal body organs) or abscesses may cause pain around the anal Fissures (ulcerated tears or cracks in the lining of the anal canal) is often associated with intense pain during defaecation. Perianal skin tags are also common in Crohn’s Disease. At the opposite end of the gastrointestinal tract, the mouth may be affected by aphthous ulcers (non-healing sores). Rarely, the oesophagus, and stomach may be involved in Crohn’s disease.
- Disease of the bile ducts and Liver Function Tests abnormality. Although the association is greater in patients affected by Ulcerative Colitis, Crohn’s Disease may also be associated with a rare condition affecting the ducts that drain the bile fluid from the liver called Primary Sclerosing Cholangitis. This condition is rare, but should always be followed up by a gastroenterologist who has experience in liver disorders.
- Gall stones. Crohn’s Disease that affects the ileum may result in an increased risk forgallstones The ileum helps absorb bile acid (resorption) which is then transported back to the liver. Disturbance is cholesterol/bile ratio increases risk for gallstones formation.
- Skin. The most common type of skin manifestation is Erythema Nodosum, which are raised areas of tender red nodules; usually appearing on the shins. Erythema Nodosum is due to inflammation of the underlying fat tissue.Another skin lesion Pyoderma Gangrenosum is much less common, is usually painful and appears as an ulcer.
- Eyes. Inflammation of the coloured ring surrounding pupil (iritis) or interior portion of the eye (uveitis), can cause blurred vision and photophobia (pain when exposed to light). Inflammation may also involve the white part of the eye (episcleritis).

- Joints disease. Crohn’s Disease is associated with an inflammatory type ofjoint disease known as seronegative spondyloarthropathy. This group of diseases is characterized by inflammation of one or more joints (arthritis) or at the points where muscles attached to bones (enthesitis). The pattern of arthritis can be grouped into large or weight-bearing joints (hips, shoulders, wrists, or elbows); or small joints of the hands and feet (often symmetrical). Less commonly, when arthritis involves the spine (ankylosing spondylitis), it causes back pain and stiffness when bending down. Our Gastroenterologists often requests or recommends involvement of expert Rheumatologists in the care of Crohn’s Disease patients who have arthritis.
- Blood clots. People with Crohn’s disease are at increased risks ofblood clots which often occur in the lower legs (deep venous thrombosis – DVT). DVT can lead to pulmonary embolism which occurs when the clot travels to the lungs, which can be fatal. Ask our Gastroenterologists for advice if you need to see a Haematologist; advice on safety of using blood thinning medications and trategies to reduce risks during situations of heightened risks eg. long overseas flights.
- Anaemia (low red cells) which can be caused by a process called Autoimmune Haemolytic Anaemia. This occurs when the immune system attacks the red blood cells causing pre-mature rupture of the oxygen carrying cells. When anaemia happens, people may have fatigue, breathlessness during exercise or a pale appearance. Anaemia can also be due to deficiencies in Vitamin B12, Folate or Iron. Specifically, the most common is iron deficiency anaemia due to blood loss (traces of blood in stools), reduced dietary intake, and persistent inflammation leading to restriction in iron absorption in the duodenum. There are many methods to supplement Iron (oral, intra-muscular injections or an infusion). Since the approval by Medicare for the use of FerInject Iron Infusion is now considered a very safe and effective way of quickly boost the body Iron stores, which helps reverse anaemia and improves symptoms of anaemia. Iron Infusions should be done in Centres where there are experienced nursing staff, and IV needle should be inserted by an experienced Doctor which drastically reduces the risk of yellow skin discolouration (caused by leakage of Iron during the infusion). Ask our staff for more information.
- Osteoporosis or thinning of the bones.Individuals with osteoporosis are at increased risk of bone fractures.
SYSTEMIC SYMPTOMS
Like many other chronic inflammatory diseases, Crohn’s Disease can cause a variety of systemic symptoms (ie. Can affecting the whole body). These include failure to gain weight in young children; growth retardation around the time of puberty as growth spurt is affected (up to 30% of children with Crohn’s disease may have retardation of growth). Fever may also be present, although it should be noted that fevers greater than 38.5 ˚C are uncommon and should always be assessed by a Doctor, as in context of Crohn’s Disease it could indicate presence of an abscess or internal organ fistulae. Amongst adults, Crohn’s Disease may manifest as weight loss, usually related to decreased food intake or loss of appetite. People with extensive small intestine disease may also have malabsorption of Carbohydrates (Fructose and/or Lactose) or lipids (fatty or oily foods), which can further exacerbate weight loss.
EXTRA-INTESTINAL SYMPTOMS
Crohn’s disease can affect many other organ systems.

Image: Iritis
CAUSE OF CROHN’S DISEASE
The cause of Crohn’s Disease is unknown, although the current thinking stipulates contribution of environmental, immune and bacterial factors in people with genetic susceptibility. About 18-20% of people with Crohn’s Disease have immediate family (a parent, a sibling or a child) with some form of IBD. Currently, more than 70 genes are thought to be involved. The first mutation found to be associated with Crohn’s was a defect in the gene called NOD2 gene (also known as the CARD15 gene), but active research is on-going into the exact mechanisms of actions of these genes.
It should be singled out that tobacco smokers are two times more likely to develop Crohn’s disease than non-smokers. Stopping smoking should be a priority for people with Crohn’s Disease, as it reduces long term complications.

Image: Gut cells in Crohn’s Disease Vs normal
Exposure to environmental triggers – possibly viruses, bacteria and/or proteins – prompts the immune system to switch on its normal defence mechanism (inflammation) against a foreign substance. The “defence” results in chronic inflammation of the intestines. In most people, this natural immune response gradually winds down once the trigger or offending substance are destroyed. In some people (possibly those with a genetic susceptibility to IBD), the immune system fails to follow the normal ‘switch off’ pathways, which thus inflammation continues.
Prolonged inflammation eventually damages the walls of the gastrointestinal tract and causes the symptoms of IBD as listed above.
PROGNOSIS
Crohn’s Disease is a chronic condition for which there is no cure. It is characterised by periods of improvement (remission) followed by episodes when symptoms flare up. With currently available treatment options, most people lead a normal lifestyle, achieve a healthy weight, and the mortality rate directly related to the disease is relatively low. As with any chronic diseases, the clinical course can vary from being benign to very severe from the onset. Some people can remain disease free for years or decades. Most people with Crohn’s live a normal lifespan, but it is important to note the disease is associated with a small increase in risk of colon and small bowel cancer. Clearly, there is a need for routine surveillance for colon cancer by colonoscopic examination and routine biopsy to detect early changes, but the interval for Colonoscopy should be discussed on an individual basis with your Gastroenterologist (depending on the severity and extent of the disease, the age at diagnosis, and whether the control of disease is achieved, and family history of colorectal cancer).
DIAGNOSIS
Crohn’s Disease can be difficult to diagnose because the symptoms can be non-specific and are similar to those of other gut disorders such as Ulcerative Colitis or Irritable Bowel Syndrome.
Your Gastroenterologist will obtain an accurate medical history, perform a careful examination, and order a series of special investigations that your General Practitioners may not have ordered. Laboratory tests and x-rays are useful, often to exclude other causes of your symptoms. Blood tests may be performed to check for anaemia, blood markers for inflammation (white cell count, an inflammation protein called CrP, and Erythrocyte Sedimentation Rate – ESR), Kidney and Liver Function Tests, Iron Vitamins levels.
Stools may be examined for occult bleeding or infection with a specific pathogen including Clostridium Difficile, E. Coli, Salmonella and Shigella. Any overseas travel should be taken into account. A special protein in the stools called Calproprectin is useful in helping diagnosing Crohn’s Disease and aid in long term follow up. Calprotectin is a protein released by a specific type of white blood cell called a neutrophil. When there is inflammation in the gastrointestinal (GI) tract, neutrophils are found in these specific areas. They release Calprotectin, resulting in an increased level in the stool. There may be out of pocket costs for this test, so ask your Gastroenterologist to obtain further information.
Colonoscopy is a powerful tool reaching an accurate diagnosis. It is often the best test for making the diagnosis of Crohn’s Disease.

Image: Colonoscope
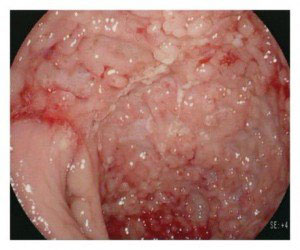
The colonoscope is a thin flexible tube that allows the Gastroenterologist to visualise the internal surface of the bowel directly. At the tip of the colonoscope, it is equipped with light source, a tiny camera and a channel to obtain biopsies (tissue sampling). With the latest advances in endoscopic systems and image processing power, the clarity and detail of the images obtained is amazing. The Gastroenterologist is able to see inflammation, ulcers, fissures (cracks in the lining of the bowel), or bleeding. Incidental polyps or benign growths can be found (most commonly in people above the age of 50), but a special type of polyps called “pseudo-polyps” can also be present. These are small masses of scar tissue that develop from granulation tissue during the healing phase in repeated cycle of ulcerations / inflammation. Pseudo-polyps themselves are thought not to be pre-cancerous growths, but the presence of pseudo-polyps often signifies long history of active disease. Patients with pseudo-polyps may require regular Colonoscopy on regular basis for polyps that have malignant potential.
You can request an appointment, or for further information, please call one of our receptionist team on 03 5941 9999.
