Colonoscopy
Colonoscopy has long suffered from a bad name, but the reputation isn’t deserved. You may feel fear, embarrassment, anger or a whole host of emotions when facing the recommendation by your doctor to have a colonoscopy. But the truth is that the vast majority of colonoscopy patients don’t have a terrible experience: the dreaded “bowel prep” has improved so much in recent years, the fasting is no longer a major issue, the sedation medicine used for colonoscopy is vastly different to 10 years ago (and yes, all patients having a colonoscopy in Australia are sedated, and you should not remember the procedure at all).
WHAT IS A COLONOSCOPY
COLONOSCOPY SHOULD BE DONE BY HIGHLY QUALIFIED SPECIALISTS
Colonoscopy is a medical procedure, and therefore should be done in an appropriate Day Surgery Centre or Hospital. You should be aware that in Australia, the fees for the doctor performing the colonoscopy are mostly covered by Medicare, but Medicare does not pay for the costs of employing highly qualified nurses, specialised automatic sterilisation machines and latest endoscopic equipment. Do not be tempted to choose where to have your colonoscopy done on the basis of costs alone. You have the right to choose to have your colonoscopy performed at highly reputable centres. Did you know that if you have Private Health Insurance, the majority of patients will have minimal or no out of pocket costs? Even if you need to pay for your medical procedure, it should be done by highly qualified Specialists in appropriately staffed centres.
In Australia, generally the doctor who performs your colonoscopy is a Gastroenterologist, a doctor who specializes in the digestive system and its disorders. Some surgeons also hold qualifications in performing colonoscopies. Make sure that your colonoscopy will be done by an experienced digestive disease specialist who is interested in constant improvement in the quality of the colonoscopy that he or she provides. Make sure your Specialist offers to be available and easily contactable after hours should you have questions, before and after the procedure.
WHY COLONOSCOPY IS PERFORMED
The two most common reasons to have a colonoscopy are to investigate symptoms that you may be experiencing (called a “diagnostic colonoscopy”); or to screen for and prevent bowel cancer (called “screening colonoscopy”). A colonoscopy is gold standard in evaluating abnormalities of the colon (including cancer, inflammation, bleeding, and polyps).
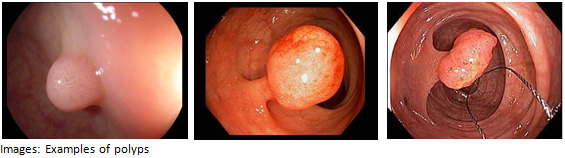
Bowel cancer refers to both colon and rectal cancer (that is, cancer that occurs anywhere in the large intestine, including the rectum). It is also often referred to as “colon cancer” or “bowel cancer”. According to the Australian Government Department of Health official statistics, more than 14,000 Australians were diagnosed with bowel cancer in 2014. Bowel cancer remains the second leading cause of cancer-related death in Australia. This is surprising as bowel cancer can be prevented, by regular routine screening and removal of silent, small, benign polyps (growths). Early detection is the key, and people with early stages of bowel cancer can be successfully treated. Recent international studies have shown that more than 90 percent of people diagnosed with stage 1 cancer (confined to the colon or rectum), survive more than five years.
WHY DO PEOPLE AVOID COLONOSCOPY
Despite the importance of colon cancer screening, people are still reluctant to get a colonoscopy. Some of the reasons people give most frequently for not getting screened include:
- “I have no symptoms”. The fact is, you may not experience symptoms of colon polyps or cancer until the polyp has grown very big. It’s always better to detect and remove polyps when they are small, as there is less risk of them transforming to cancer, much easier for the Gastroenterologist to remove and hence less risks such as bleeding or infection, and less time under sedation. Furthermore, screening is aimed at detecting early cancer, and the earlier the detection, the easier the treatment.
- “I am concerned about safety”. In Australia, more than 500,000 colonoscopies are performed each year. Keep this fact in mind: colonoscopy is a common and generally safe procedure, although nothing is without risk, and colonoscopy is no different. That’s why you need to ensure your colonoscopy is performed by highly qualified Specialists and in appropriate Day Surgery Centre/hospital. You should not choose where to have colonoscopy based on costs alone.
- “I am embarrassed by the procedure”. Your privacy is of the utmost concern to your treating Gastroenterologist, our affiliated facilities and our staff. Taking a positive step in caring for your health should outweigh the potential embarrassment anticipated.
- “I don’t like the bowel prep and fasting the day before”. This statement is fairly accurate, but much has changed in the last 5-10 years. The volume of the medicine you are required to drink is generally 2-3 drinks of 250mL (about the same as a cup of coffee). Ask our staff about the new prep medicine that is easier to take. If you have your colonoscopy done at one of our facilities, you will be told the exact time to arrive, and can drink lots of water up until 6 hours prior to arrival time; and can have small sips of water or suck on ice cubes until 3 hours prior to your arrival. Being “dehydrated” is much less likely if you following our instructions.
- “I am scared of the pain”. All colonoscopies in Australia should be done under sedation. Our Gastroenterologists are skilful and are very well trained. The procedure may involve modest discomfort, as a small amount of air is used to inflate the colon to help the doctor see better, but the air will slowly be absorbed and you should be able to pass the air. You will sleep through the entire examination, and it is not unusual for people to wake up and wonder if the colonoscopy has been done!
- “My doctor hasn’t recommended colonoscopy”. Believe it or not, considering the importance of screening and preventing bowel cancer, many doctors still don’t make a point of recommending the procedure. If your doctor hasn’t had the discussion with you if you are 50 or over, you are allowed to politely start the conversation yourself, much like asking about Pap Smear test or mammography in the appropriate group of people.
THE RISKS
Colonoscopy is medical procedure, and like all medical procedures, it is not risk free. Much can be done to minimise the risks, and in the vast majority of patients the benefits of cancer prevention outweigh the risks. Potential risks of colonoscopy may include bleeding, infection, intestinal perforation (a small tear in the bowel), missing polyps or cancer, and adverse reactions associated with sedation medicine or colonoscopy preparation fluids. Many of these risks rarely occur and are even less common with a colonoscopy that doesn’t involve polyp removal. In general, the bigger the polyps, the higher the risks. Therefore, it is preferable to have routine colonoscopies, as it is more likely that small polyps are picked up early. You can reduce risks by ensuring that the doctor that performs the procedure is an experienced Gastroenterologist or surgeon. All our Gastroenterologists are very well trained, diligent and careful. Another great way to reduce procedural risk and increase the detection of polyps is to arrive at your procedure with a clean colon. This can be done by following our instructions, which will be sent to you in the mail or you can download here. The most common adverse events associated with colonoscopy preps include bloating, nausea, abdominal pain and vomiting. Rarely, more serious risks have occurred as well and you can find further information about the risks and adverse events associated with the prep for a colonoscopy in the “information leaflet” supplied by their manufacturers and from your pharmacy. As certain medical conditions may affect these events, you should fully discuss these, as well as your prep, and how to properly take it with your treating Gastroenterologist.
WHAT ARE THE FINANCIAL COSTS
The costs associated with a colonoscopy vary, but at our facilities, doctors associated fees are covered by Medicare including the anaesthetist and histopathologist. There may be fees for your specialist gastroenterologist. Medicare does not pay for the costs of nursing staff, sterilisation, and endoscopy equipment (the “hospital fee”). If you have Private Health Insurance, hospital fees are covered to varying degrees, depending on your chosen level of cover and your choice of excess with a particular health fund. If you do not have Private Health Insurance, you can contact our office and enquire about the out-of-pocket costs depending on whether you hold a valid Pension or Health Care Card. It is important that you do not base your decision where to have your colonoscopy performed purely on the basis of costs, as you would want to have it done in reputable centres. Remember the best centre(s) have the best equipment and employ the best nursing staff to look after you during and after the procedure.
PREPARING FOR COLONOSCOPY
After being recommended to have a colonoscopy, ask our staff what the procedure is, who will be performing it, and what you need to do before and after the procedure. You can ask for the Hospital Admission paperwork to be emailed to you, have it posted out or download here. You may need a detailed conversation on how best to ensure a clear colon so that your Gastroenterologist can accurately and carefully look for small polyps. One of the nurses at our centre will call you before your admission when your paperwork is received by us. Make sure you have clearly filled out your medical history and conditions, as well as the medications you are taking, including blood thinners of any type, epilepsy and diabetes medications, use of CPAP machines (if you have Obstructive Sleep Apnoea), or if you have a heart pace maker / defibrillator — this information needs to be provided to your Anaesthetist and Gastroenterologist who will make recommendations if any medications need to be stopped or dosages adjusted prior to your procedure.
MAKING ARRANGEMENTS
Part of planning for your colonoscopy entails getting all the details down. While the colonoscopy itself is just a short part of one day, you need to take care of certain things ahead of time.
Read through the complete instructions and information provided by our administration team. If you have not received it, you can download the Bowel Prep Instruction Sheet, or have it faxed, emailed or posted to you again. You can also attend our office to pick up both the instruction sheets and the bowel prep medicine so that you don’t have to find the medicine at your chemist. Make sure you fully understand all the information and instructions before you start your bowel preparation. If you previously had a bad reaction such as abdominal pain, nausea and vomiting with the bowel prep, contact our office to ask is there anything you can do to reduce the chance if happening again. Some people who have had previous colonoscopy, and have been told that their bowel prep is “sub-optimal”, if this is the case, ask us if our Gastroenterologist recommend one or two extra sachets of the bowel prep medicine to help improve the views this time.
Most people can work until 3:00pm the day before the scheduled colonoscopy, but you need to arrange for the entire day of the procedure off work. You will be sedated, so you’ll be groggy and your reaction time will be slower. Don’t book important appointments on the day of your procedure, and most patients are fine to return to work the day after their procedure.
Schedule a ride. You will be required to have someone to accompany you and drive you from the centre where your colonoscopy is performed. The facility rules (and liability laws) don’t allow you to leave or drive yourself home, and you can’t take a taxi or bus home by yourself. Ideally, you should have someone who can spend the rest of the day with you at home as well. It may be an inconvenience, but for your own safety you will need a friend or family member there with you when being discharged.
REMOVING POLYPS AND DOING BIOPSIES
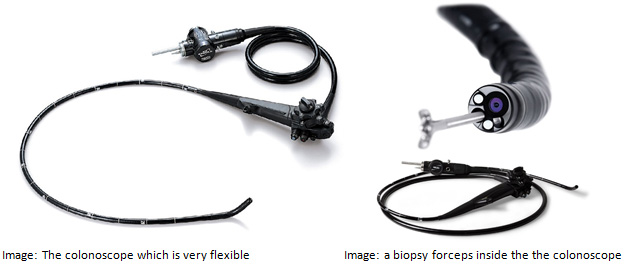
During the course of your colonoscopy, your Gastroenterologists will use air or medical Carbon Dioxide gas to inflate the colon to help see the lumen. If your Gastroenterologist sees a polyp (benign growth) or other abnormalities, he or she may remove it in its entirety or a piece of it if it’s too big to safely be removed with a colonoscope.
The equipment used includes biopsy forceps or a snare. You can see that there is a channel at the tip of the colonoscope. Most colonoscopes have multiple channels — it is through the channels that your Gastroenterologist can utilise the equipment to remove the polyps.
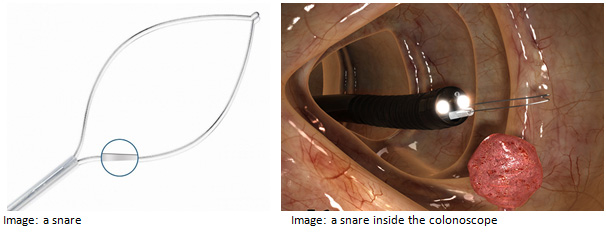
Tissue during the colonoscopy is removed in two general ways:
- Polypectomy: a tweezer like instrument called forceps or a flexible wire loop called a snare can be passed through the colonoscope to cut out the polyp. Either of these methods can be used “cold” or “hot”. Hot means with the use of cautery or heat to burn the tissue as the polyp is being removed.
- Biopsy: In a biopsy, particularly when the doctor finds a large polyp, he or she removes a small amount of tissue for the lab to examine and determine its microscopic nature. This is called a “biopsy”. When knowing the nature of the polyp, your Gastroenterologist can plan for definitive removal and future treatment.
WHY ARE POLYPS OR TISSUE SENT TO THE LABORATORY
After removing a polyp, your Gastroenterologist will retrieve and send the tissue to a laboratory to determine the nature of the lesion. Most colon cancer starts as noncancerous polyps. Because the underlying nature of colon polyps can’t be determined without being examined under a microscope by an experienced Histopathologist, most polyps are removed during colonoscopy. The colon doesn’t feel pinching or burning sensations, and as patients are sedated, people don’t feel a polyp being removed. The colon pain receptors do feel the stretching sensation from air distension, but your Gastroenterologist will try to remove most of the air inside the colon (by suctioning) before completing the procedure.
AFTER REMOVAL OF POLYPS
When a polyp is removed from the lining of the bowel, a small ulcer or sore remains at the removal site, which can be prone to bleeding, either immediately or within two weeks (called “delayed bleeding”). If you had polyps removed during your colonoscopy, your Gastroenterologist may specifically request withholding blood thinning medications or advising against alcohol consumption for a certain number of days. Ask your doctor if he or she wants you withhold any medications, and when it is safe to resume taking your normal medicines. Some over-the-counter medicines may increase the risks of bleeding post procedure, and you should ask your Gastroenterologist if you can continue to take them.
Within 30-40 minutes after the procedure or when you are fully awake, your doctor will be able to reassure you; or advise you whether there was something serious or concerning detected on the examination. You will be provided with a written report which contains photos of the large bowel taken during the examination. A copy of the report will be sent to your Family Doctor, either via email or by post on the same day. The majority of individuals undergoing colonoscopy get reassuring news that the examination was normal or that only small polyps were found which had been safely and successfully removed. If your Gastroenterologist is concerned about something found during the examination, the doctor will request you to return – usually within a week or two to discuss the laboratory results.
Waiting for results of biopsies can be unnerving. Be sure you or your family member driving you home gets a chance to review the report of the colonoscopy with your doctor before you leave the endoscopy centre. Knowing whether you have something to be concerned about, or your doctor doesn’t want to see you for 5-10 years will be reassuring. Don’t spend too much time worrying about biopsy results, but be comforted by the fact that you took the proper steps for your health by getting a colonoscopy, and that you will take the proper steps for what happens next. The results may simply show an advanced polyp that may have been caught in time, and if colon cancer does occur, it’s curable when caught early. Doctors continue to discover more about colon cancer and the factors that influence its development, and as you’re finding out, they also have effective screening tools that aid in its prevention.
COMMONLY ASKED QUESTIONS
Why Do I Need to Get a Colonoscopy?
The simple answer is: Getting a colonoscopy can save your life. A colonoscopy can detect and remove polyps before they develop into colon cancer. It remains the best tool for doctors to detect early polyps (far and above CT scanning or stool testing for blood), and remove them. It can also detect early stage colon cancer, if present, so it can be identified while still highly treatable. If you’re 50yrs or older (or younger, with the risk factors discussed in Bowel Cancer section), and have never had a screening colonoscopy, it’s time. A common, simple procedure could save your life. Close to 500,000 colonoscopies are performed each year in Australia.
More than 90 percent of people diagnosed and treated when the cancer (stage 1) is confined to the colon or rectum survive more than five years. According to experts in the United States, 60 percent of deaths from bowel cancer could be prevented if everyone age 50yrs and older were screened regularly.
When Should I Get My First Colonoscopy?
There are two types of colonoscopy:
- Screening colonoscopy. This refers to colonoscopy when you have no symptoms. This should be done when you reach the age of 50, even if you don’t have any symptoms. People with risk factors may need to start at a younger age, including
- People who have a close relative with bowel cancer – mother, father, a brother or a sister;
- Individuals with previous colonic polyps;
- Individuals with bowel conditions called Crohn’s Disease or Ulcerative Colitis.
- Diagnostic colonoscopy, which is requested by your Family Doctor or Gastroenterologist when you have certain symptoms or signs of potential colorectal polyps or other inflammatory conditions. A diagnostic colonoscopy may be necessary at any age, to find out the cause of a specific symptom.
How Often Do I Need to Get a Colonoscopy for Bowel Cancer Screening?
The good news is that, under normal circumstances, you only have to undergo a screening colonoscopy every 7-10 years if the previous examination was normal and you don’t have any other risk factors for bowel cancer. And, who knows, by the time you need your next one, the Pharmaceutical companies may have figured out how to make the bowel prep taste good. For individuals with an increased risk of colon polyps or cancer, the interval for colonoscopy can be shorter. Your Gastroenterologist will provide you with the recommended interval based on the specific risk factors you may have, the number of polyps removed, the size of the polyps and the laboratory grading.
How Long Does the Procedure Take?
At our centres, most patients will be advised a specific time to arrive which is about 30 minutes prior to the procedure to change clothes and get admitted to the pre-procedure room. This will allow you to plan the day, and to arrange someone to pick you up. Many people are surprised at how quickly the actual procedure flies by. Maybe it’s the new sedation medicine that is now widely available, maybe it’s just that the procedure is really not that big a deal after all. It generally takes less than half an hour, and you most likely won’t notice the time going by as you will receive light sedation. You will find overall you will be at our centre for approximately 2hrs in total on the day of your procedure.
Is a Colonoscopy painful?
Not generally… that’s the aim of your Anaesthetist and Gastroenterologist. Unlike many other countries, all patients (except for rare circumstances) undergoing colonoscopy in Australia should be given sedation to make them very comfortable during the examination. Because the colon is folded in many parts, the doctor will need to use air to inflate it to ensure optimal views of the entire colon. The air may cause you to feel a little bloated after the procedure, and it is normal to let it pass. The nursing staff will provide you with a list of written discharge instructions including what symptoms may be normal after colonoscopy and what symptoms should prompt you to call the centre or your doctor. Even after hours and on weekends, one of our Gastroenterologists will always be available to discuss or give over the phone advice should you have concerning symptoms such as pain or excessive bleeding. It is part of our high quality service, and people in Australia should demand this service from their doctor wherever they choose to have their colonoscopy.
What Happens if the Doctor Finds Something Abnormal?
If your Gastroenterologist finds one or more polyps during the procedure, he or she can remove the majority of them right then and there using specialized tools called biopsy forceps or snares, which can be fed through a channel inside the colonoscope. If a polyp or tumour is too big to be safely removed through the colonoscope, the doctor will take small samples the tissue (biopsy) to send to a lab to be examined by an experienced Histopathologist. If other abnormalities are found in the colon, or the colonoscopy is being done to determine the cause of symptoms, biopsies can also be performed. It usually takes no more than a few days to get the results of a biopsy. One of our reception staff will call you to let you know if your doctor wants to discuss the results with you in person, although in most instances the news is good.
How Long Should I Be Off Work?
It may be recommended that you finish work at 3pm the day before your scheduled colonoscopy, and you will need to arrange to take the entire day of the procedure off work. Most people wake up well within 30 minutes after the completion of the colonoscopy. Initially, you may feel groggy from the sedation medicine. For this and legal reasons, you won’t be allowed to leave the recovery room alone or drive any vehicle or operate any machinery until the next morning, so line up a ride ahead of time. Ask your doctor if you need a medical certificate as you will need to take the rest of the day off. We find that if you relax at home with some light food and lots of fluids and get a good night’s sleep you will be ready to go to work the next morning.
For further advice and information, you can request an appointment, or call one of our receptionist team on .
Useful links:
http://www.jodileefoundation.org.au
http://www.cancerscreening.gov.au
National Bowel Cancer Screening hotline 1800 118 868

